Abstract
Introduction: Due to improvements in comprehensive medical care, data suggests that about 93% of children born with sickle cell disease (SCD) are now living past 18 years of age. Young adulthood is a high-risk time for clinical complications and progressive SCD-related organ damage. The majority of SCD-related deaths occur after 18 years of age and after transfer to an adult provider, which leaves this population particularly vulnerable to poor outcomes. In addition, current research suggests that this transition period is associated with increased health care utilization (HCU), and thus, highlights the need for proper care models for transitioning SCD patients. This study aims to describe the pattern of HCU and health quality indicators (HQI) in SCD patients at different ages of the transition period.
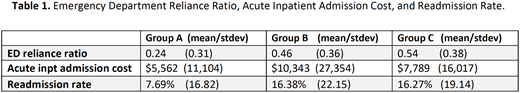
Methods: A retrospective data analysis of health insurance claims from a single health plan for service dates 04/01/2016 through 03/31/2017 was conducted. Members meeting the claims-based definition of SCD (those with any sickle cell related ICD 9/10 CM diagnosis code on at least two separate encounters on distinct dates during the study period) with 12 months of continuous membership were included in the initial sample. Those within this sample that are 11-35 years old were selected and further stratified into three groups representing pre-transition (Group A: 11-18 yr.), transition (Group B: 19-26 yr.), and adult (Group C: 27-35 yr.). Data obtained include demographics, HCU patterns (emergency department (ED) visits, frequency of acute inpatient admissions and diagnosis, 30-day readmission rate and total cost of care), and HQI (hydroxyurea (HU) use, influenza (Flu) vaccination status, and total cost and number of visits for PCP and specialists). Two specific metrics of utilization included in the analysis were emergency department reliance ratio (EDR) and calculated HU medication possession ratio (MPR). EDR was calculated as the sum total of all ED visits divided by the total number of ambulatory visits. An EDR ≥ 0.33 was considered an indicator of excessive reliance. MPR was calculated as total days of HU prescription divided by the difference between the number of days of insurance enrollment and the number of days hospitalized. MPR of 1.0 was considered complete adherence.
Results: A total of 144 members, 88 (61%) female, fit the inclusion criteria. Member number was similarly distributed in all groups: A: 50, B: 48, and C: 46. Medicaid was the primary insurance for 123 (85%) patients, followed by Commercial 15 (10%), and Medicare 6 (5%). While average total cost of care was similar in the three groups (A: $22,688; B: $25,525 and C: $25,873) average cost of ED visits was three times more for Group C: $2,153 as compared with A: $862 and B: $954. As shown in table 1, an increase in EDR, acute inpatient admission cost, and readmission rate was noted between groups A and B. Moreover, although Group C represented older patients, their ED utilization, EDR, and readmission rate were comparable with that of Group B. Analysis of HQI showed that almost half (44%) of the patients in Group A had no ED visits during the study period as compared to 29% of Group B and 26% of Group C. Of note, Group C had a higher number of 10 or more ED visits (n=9; range 10- 63 visits) compared to Group B (n=2; range 1-14) and Group A (n=1). More than 50% of patients in Groups B and C did not have a PCP or specialty visit within the study period vs. 25% in Group A. Group B had 13 visits to pediatric Heme/Onc providers, but no visits to adult Heme/Onc providers, even though the institutional maximum transition age is 21 years old. MPR was roughly 0.25 for each of the groups, and thus, consistent with poor adherence across all ages. Influenza vaccination was less frequent in the transition group (Group B) than in Groups A and C.
Conclusion: Our data shows the vulnerability of SCD patients during their transition years (19-26 yr.) from pediatric to adulthood, thereby confirming the findings from prior studies. These patients demonstrated higher HCU patterns (i.e. EDR, acute inpatient admission cost and readmission rate) and lower HQI (i.e. lack of PCP and Heme/Onc visits, lower Flu vaccinations, and MPR). Thus, this study highlights the urgent need of improved protocols and systems in order to provide continuity and quality care during these critical transition years.
"The last two authors of this abstract contributed equally."
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal